Understanding MASLD: A Closer Look at Fatty Liver Disease
One of the most common causes of fatty liver disease is known as Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD). MASLD is characterized by accumulation of fat in the cells of the liver along with at least one risk factor associated with metabolic dysfunction, such as diabetes or obesity.
MASLD comprises a spectrum of stages. The early stage is characterised by fat in the liver. The condition may progress to cause inflammation with damage to the cells of the liver. Over time, this may lead to scarring (liver fibrosis), which if left untreated, may become irreversible, leading to liver cirrhosis. Irreversible scarring of the liver can eventually lead to liver failure. Majority of individuals with MASLD will remain in the first stage, with only approximately 20% progressing to the stage of inflammation (with or without scarring), and even less progressing to the more advanced stages.
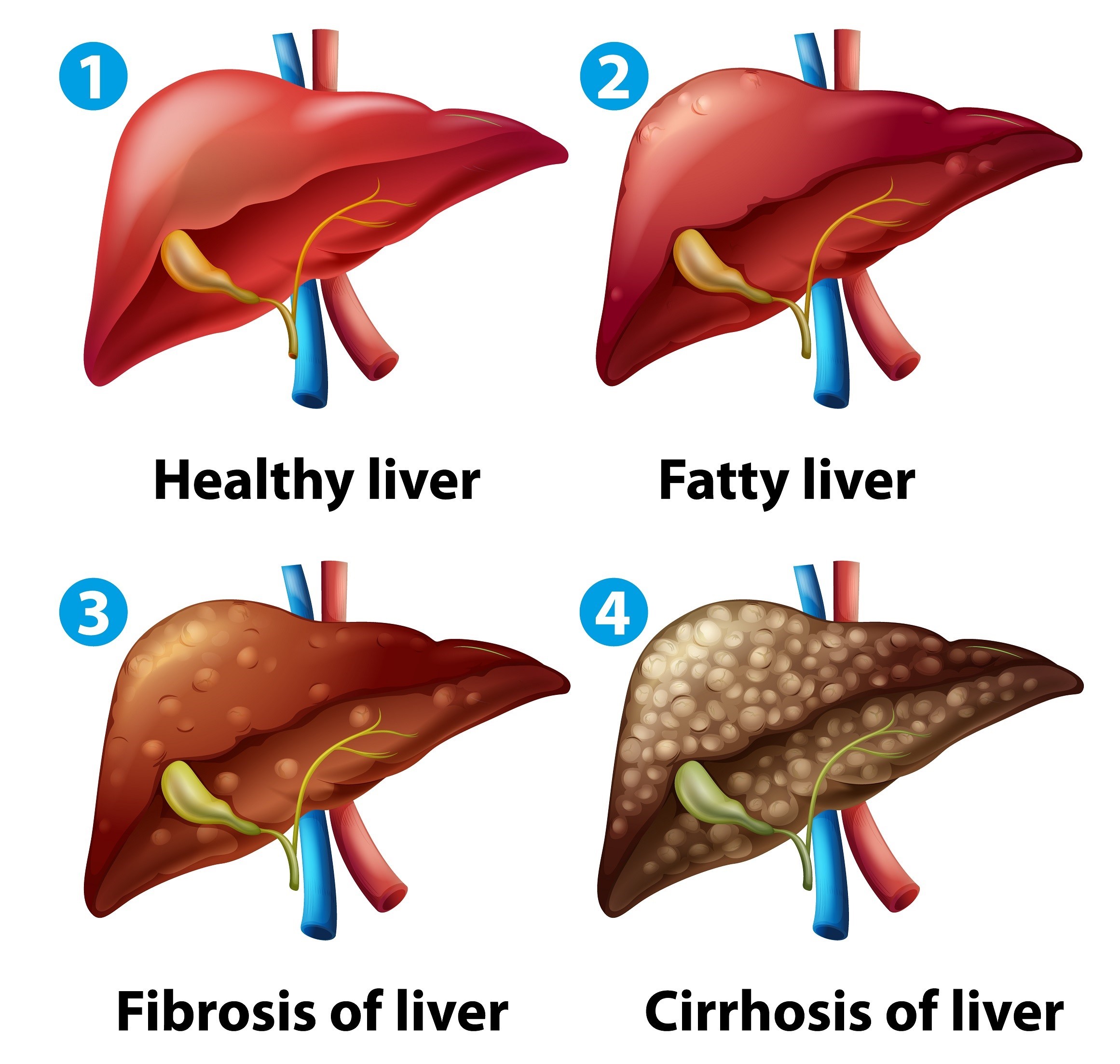
Stages of MASLD
1) Fat deposition in the liver - at this stage, there is no damage to the liver, and this can be completely reversed.
2) Metabolic dysfunction-associated steatohepatitis (MASH) with mild fibrosis - at this stage, there is liver inflammation causing some damage to the cells of the liver. As the damage is repaired, it can start to cause mild liver fibrosis (scarring). MASH in the early stages is reversible.
3) MASH with moderate Fibrosis - as the damage from liver inflammation progresses, scarring will also progress. MASH with moderate fibrosis is usually still reversible.
4) MASH with advanced Fibrosis – the fibrosis can progress to more advanced stages. At this stage it may still be possible to reverse some of the damage, but it is important to stop further damage to prevent development of liver cirrhosis.
5) Liver Cirrhosis – as the scarring becomes severe, it can become irreversible and changes the shape of your liver. At this stage, your liver is unable to function adequately, and it can eventually lead to liver failure.
MASLD is now the most common cause of chronic liver disease globally and is currently estimated to affect up to 38% of the adult population worldwide, with higher rates in the Middle East and North Africa (MENA) region, affecting over 42% of the adult population.
About 20% of individuals with MASLD will develop MASH; however, individuals with type 2 diabetes or obesity are more likely to progress to MASH.
What are the main risk factors for developing MASLD?
- Type 2 diabetes.
- Obesity or increased waist circumference.
- Overconsumption of calories.
- Diets high in meat, saturated fat, ultra processed foods and refined sugars.
- Low levels of physical activity.
Other conditions associated with MASLD
- High blood pressure
- Abnormal lipid profile on your blood test
- Obstructive Sleep Apnoea
- Polycystic Ovarian Syndrome (PCOS)
Diagnosis
The diagnosis of MASLD is based on the presence of fatty liver as well as at least one of the following five risk factors listed in the table below.
| Cardiometabolic Risk factors |
|---|
| Overweight or an increased waist circumference |
| Diabetes or pre-diabetes |
| Raised blood pressure (blood pressure ≥ 130/85 mmHg or on treatment for high blood pressure) |
| Raised levels of triglycerides |
| Low levels of HDL cholesterol |
Your doctor will do a range of blood tests including your liver function tests, which may reveal raised liver enzymes. However, it is important to note, your liver tests can remain normal despite having MASLD.
If you are considered at risk for the development of liver fibrosis due to MASLD, your doctor can perform a fibrosis risk score based on your blood tests and this will help guide further management.
- To diagnose MASLD as your cause of fatty liver, your doctor will exclude other causes, such as increased consumption of alcohol, viral hepatitis, certain medications etc.
- In individuals consuming high levels of alcohol, the condition is termed alcoholic-related liver disease (ALD). Individuals with a history of moderate levels of alcohol intake, alongside a metabolic risk factor will have a mixed picture.

Symptoms of MASLD
Most people with MASLD will have no symptoms or physical signs in the early stages.
If symptoms occur, this may include fatigue or a dull ache in the right upper abdomen. Once the condition has progressed to the more advanced stages, such as liver cirrhosis, some of the symptoms may include nausea, vomiting, jaundice, ankle swelling, swelling of the abdomen, itching, easy bruising, dark urine and shortness of breath.
Fatty liver is frequently incidentally picked up on an abdominal ultrasound performed for another reason and may be the first sign of the condition.
Why is it crucial to prevent the progression of MASLD?
As MASLD progresses, it is associated with an increased risk of liver failure, heart disease, chronic kidney disease, liver cancer and other cancers.
If you have been diagnosed with MASLD, what can you do to reverse it and/or prevent progression?
- Weight Loss
- Dietary modifications
- Physical activity
- Avoid Alcohol
- Smoking cessation
- Manage your current health conditions
1) Weight Loss if you are overweight
- Reduction of 5% or more of total body weight will reduce liver fat.
- Reduction of 7-10% of total body weight will improve liver inflammation.
- Reduction of 10% or more of body weight with improve scarring in the liver.
Individuals in the normal weight category will still benefit from 3-5% reduction of total body weight to reduce liver fat.
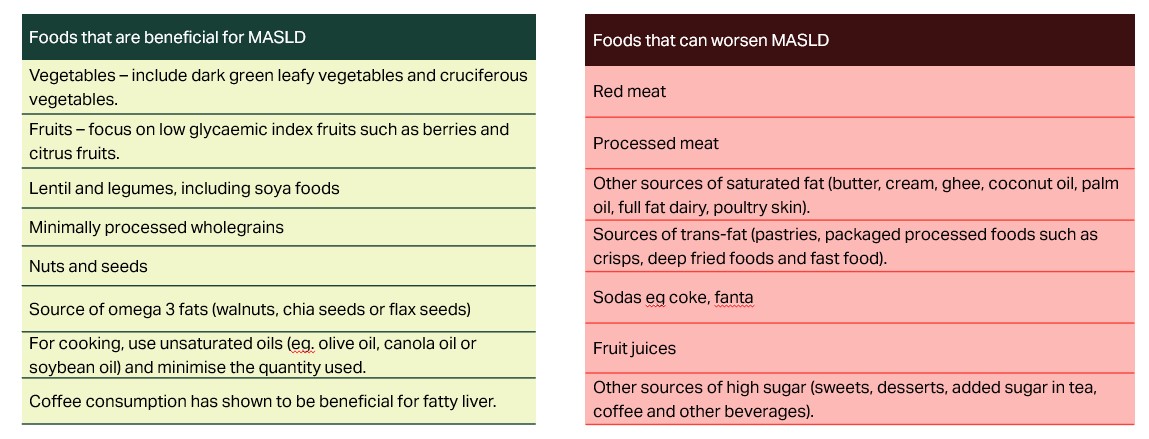
2) Dietary modifications
Consumption of a healthy plant-predominant diet has been shown to help improve fatty liver and can also aid in weight loss. Individuals that are consuming a plant-predominant diet, should supplement with vitamin B12.
3) Physical activity
A combination of aerobic and resistance training will improve liver fat and will also improve insulin resistance in individuals with diabetes or prediabetes. Additionally, physical activity has been shown to reduce visceral fat, improve body composition, reduce triglycerides and increase HDL cholesterol (good cholesterol).
Avoid Sedentary time – In addition to structured physical activity, it is important to find opportunities for movement throughout the day: take the stairs instead of elevators, try a standing desk, and consider walking meetings. Break up prolonged periods of sitting at least every 60 mins with short bouts of walking.
4) Avoid Alcohol
Studies have shown that even low to moderate levels of alcohol consumption can increase the risk of progression of MASLD to the more advanced stages. If you have fatty liver disease, there is no safe limit for alcohol consumption, and it is best to avoid alcohol completely.
5) Smoking cessation
Smoking is associated with an increased risk of MASLD and the risk of progression to scarring and the development of liver cancer.
6) Manage your current health conditions
Optimise management of associated conditions including diabetes and high blood pressure.
Lifestyle interventions are crucial in the prevention and even reversal of the condition in the early stages. All individuals with MASLD or at risk of developing it, should be assessed by their doctor for further management and investigations.
Any questions?
If you have any questions or comments, please write to us on employeebenefits.mea@howdengroup.com
References
- Younossi, Zobair M. et al. Global Consensus Recommendations for Metabolic Dysfunction-Associated Steatotic Liver Disease and Steatohepatitis. Gastroenterology, Volume 0, Issue 0
- EASL–EASD–EASO Clinical Practice Guidelines on the management of metabolic dysfunction-associated steatotic liver disease (MASLD). Tacke, Frank et al. Journal of Hepatology, Volume 81, Issue 3, 492 - 542
- Marti-Aguado, David et al. Low-to-moderate alcohol consumption is associated with increased fibrosis in individuals with metabolic dysfunction-associated steatotic liver disease. Journal of Hepatology, Volume 81, Issue 6, 930 - 940
- MASLD: a systemic metabolic disorder with cardiovascular and malignant complications | Gut (Gut BMJ)
- MASLD, NAFLD and fatty liver disease - British Liver Trust
Disclaimer:
The content in this article is for general informational purpose and is not meant to replace or substitute for professional medical advice, diagnosis or treatment. Always consult a qualified healthcare professional with any questions or concerns about your health.